Blisterata, a term used to describe various blistering skin disorders, manifests as the formation of fluid-filled blisters on the skin’s surface. These blisters can range in size from small vesicles to larger bullae. Blisterata encompasses a spectrum of conditions, each with its own unique etiology and clinical presentation. While some forms of blisterata may be acute and self-limiting, others can be chronic and significantly impact an individual’s quality of life.
Causes and Risk Factors
Blisterata can arise from a multitude of causes, including autoimmune reactions, genetic predisposition, infections, environmental factors, and medications. Autoimmune blistering disorders, such as pemphigus vulgaris and bullous pemphigoid, occur when the immune system mistakenly targets proteins within the skin, leading to blister formation.

Infections caused by pathogens like herpes simplex virus (HSV) or varicella-zoster virus (VZV) can also trigger blisterata. Additionally, exposure to allergens or irritants, such as certain chemicals or plants like poison ivy, can induce contact dermatitis and blister formation.
Types of Blisterata
Blisterata encompasses several distinct types, each with its own pathophysiology and clinical characteristics:
- Contact Blisterata: Contact dermatitis results from direct exposure to irritants or allergens, triggering an inflammatory response in the skin and the subsequent formation of blisters. Common irritants include harsh chemicals, detergents, and certain metals, while allergens may include latex or certain plant extracts.
- Autoimmune Blisterata: Autoimmune blistering disorders occur when the immune system mistakenly targets proteins within the skin’s structure, leading to the formation of blisters. Examples include pemphigus vulgaris, characterized by the presence of intraepithelial blisters, and bullous pemphigoid, which typically presents with subepidermal blisters.
- Infectious Blisterata: Infectious agents, such as viruses or bacteria, can cause blisterata through direct invasion of the skin or by triggering an immune-mediated response. Herpes simplex virus (HSV) infections can lead to the development of herpetic lesions, characterized by painful clusters of vesicles, while varicella-zoster virus (VZV) causes chickenpox and shingles, both of which present with vesicular rashes.
Symptoms and Diagnosis
The clinical presentation of blisterata varies depending on the underlying cause and specific type of blistering disorder. Common symptoms include the presence of fluid-filled blisters, erythema, itching, burning sensations, and pain.
also read: Top Firearms for Novices: A Beginner’s Guide
Diagnosis often requires a comprehensive evaluation, including a detailed medical history, physical examination, and, in some cases, skin biopsies or laboratory tests. Direct immunofluorescence studies can help differentiate between various autoimmune blistering disorders by identifying specific immunoglobulins and complement proteins within the skin.
Treatment Options
The management of blisterata aims to alleviate symptoms, promote healing, and prevent disease progression. Treatment options may vary depending on the underlying cause and severity of the condition:
- Medications: Systemic corticosteroids are often used as first-line therapy for autoimmune blistering disorders to suppress the immune response and reduce inflammation. Immunosuppressive agents, such as azathioprine or mycophenolate mofetil, may be prescribed for refractory cases or to minimize long-term steroid use. Antiviral medications, such as acyclovir or valacyclovir, can effectively treat herpes simplex virus (HSV) infections and reduce the frequency and severity of recurrent outbreaks.
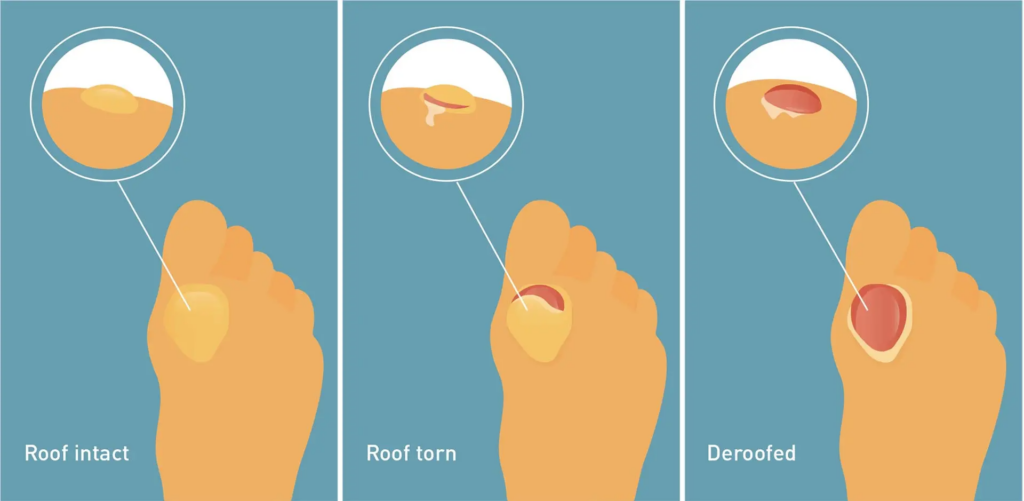
- Topical Treatments: Topical corticosteroids, calcineurin inhibitors (e.g., tacrolimus or pimecrolimus), or emollients can provide symptomatic relief and promote wound healing in localized blistering lesions. Non-adherent dressings or hydrocolloid dressings may be applied to protect fragile blistered skin and prevent secondary infection.
- Surgical Interventions: In severe cases of blisterata, surgical interventions such as debridement, drainage of large bullae, or excision of affected skin may be necessary to facilitate wound healing and prevent complications such as infection or scarring.
Management and Prevention Strategies
Managing blisterata involves a multifaceted approach aimed at minimizing disease activity, preventing exacerbations, and improving quality of life. Strategies may include:

- Lifestyle Modifications: Avoiding known triggers such as allergens, irritants, or environmental factors that can exacerbate blistering episodes. Maintaining good skincare practices, including gentle cleansing and moisturizing, can help protect the skin barrier and reduce the risk of flare-ups.
- Avoidance of Triggers: Identifying and avoiding potential triggers, such as specific foods, medications, or environmental allergens, can help prevent recurrent blistering episodes. Patch testing may be performed to identify allergens responsible for contact dermatitis and guide avoidance strategies.
- Immunizations: Vaccination against infectious agents known to trigger blisterata, such as herpes zoster virus (HZV), can help prevent primary infection or reduce the risk of recurrent outbreaks. The herpes zoster vaccine, which contains live attenuated virus particles, is recommended for individuals aged 50 years and older to reduce the risk of developing shingles and its associated complications.
Coping with Blisterata
Living with blisterata can have significant physical, emotional, and psychosocial impacts on affected individuals. Coping strategies may include:

- Support Groups: Joining support groups or online communities where individuals with blistering skin disorders can share experiences, coping strategies, and emotional support can provide a sense of community and solidarity.
- Psychological Support: Seeking counseling or therapy from mental health professionals experienced in managing chronic skin conditions can help individuals cope with the emotional and psychological aspects of living with blisterata. Cognitive-behavioral therapy (CBT) techniques, relaxation exercises, and stress management strategies may be beneficial in reducing anxiety, depression, or social isolation associated with the condition.
Complications and Long-Term Outlook
While most cases of blisterata can be effectively managed with appropriate treatment and lifestyle modifications, complications may arise, particularly in severe or recalcitrant cases. Potential complications include secondary bacterial infections, scarring, pigmentary changes, and psychosocial impairment. The long-term outlook for individuals with blistering skin disorders varies depending on the underlying cause, disease severity, and response to treatment.
also read:Understanding FTMÇ – A Complete Guide
Regular follow-up with healthcare providers, adherence to treatment regimens, and proactive management of comorbidities are essential for optimizing outcomes and minimizing disease-related morbidity.
Current Research and Future Directions
Ongoing research efforts aim to advance our understanding of the pathogenesis, diagnosis, and treatment of blisterata. Future directions may include the development of novel therapeutic agents targeting specific molecular pathways involved in autoimmune blistering disorders, the exploration of biomarkers for disease activity and treatment response, and the investigation of personalized medicine approaches tailored to individual patient characteristics.
also read: GM Salary Building Technology and Ideas BD In 2024
Collaborative research initiatives involving multidisciplinary teams of clinicians, scientists, and patient advocates are essential for driving innovation and improving outcomes for individuals affected by blistering skin disorders.
Conclusion
Blisterata encompasses a diverse group of skin disorders characterized by the formation of blisters on the skin’s surface. While these conditions can be challenging to manage, advances in understanding their underlying mechanisms and treatment options have led to significant improvements in patient care and outcomes. Through a comprehensive approach involving medical therapy, lifestyle modifications, and psychological support, individuals with blistering skin disorders can effectively manage their condition and lead fulfilling lives.
Frequently Asked Questions
What are the common triggers for blisterata flare-ups?
Common triggers include allergens, irritants, infections, genetics, hormonal changes, and environmental factors like sun exposure or friction.
Is blisterata contagious?
It depends on the cause. Viral blisterata, like herpes, can be contagious through direct contact, while autoimmune forms are not.
How can I prevent blisterata flare-ups?
Avoiding triggers, maintaining good skincare, protecting from sun exposure, managing stress, and following treatment plans can help prevent flare-ups.
Are there dietary changes that can help manage blisterata?
Some find relief by avoiding dairy, gluten, processed foods, sugar, or saturated fats, but consult a healthcare professional first.
Can children develop blisterata?
Yes, they can. Some conditions, like bullous impetigo or eczema herpeticum, are more common in children.